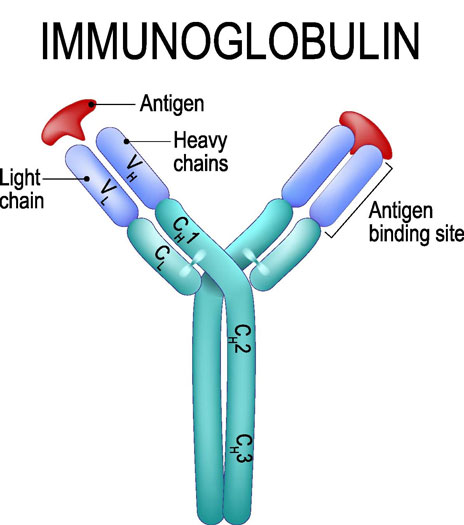
Monoclonal antibodies are those antibodies that target a specific (single-source) antigens.
Due to this specificity, these antibodies are used in clinical therapy to treat diseases like cancer.
This is called immunotherapy and is quite effective with minimal side effects.
Hence, the use of monoclonal antibodies is gaining importance.
A Brief Background
Advancements in cell biology have led to the fusion of different cells to form a “hybrid’ cell.
These hybrid cells express the properties of both parental cell lines.
The clone derived from the fusion of a single differentiated B-cell (antibody-forming) is a clone of a single B-cell.
This clone produces antibodies of a single specificity.
Therefore, such antibodies are known as monoclonal antibodies. All molecules of a monoclonal antibody will have the same specificity.
In 1975, two scientists, Georges Kohler and Cesar Milstein, devised a revolutionary method for preparing monoclonal antibodies.
This quickly became one of immunology’s key technologies, and they were awarded the Nobel Prize for the same in medicine and physiology in 1984.
Production of monoclonal antibodies
Monoclonal antibodies are produced by either of the two methods.
- In Vitro Methods (Using cell lines in glassware)
- In the Vivo method (Using living animals like Mice).
In Vitro Method
- In this method, the monoclonal antibodies are produced by fusing usually activated antibody-producing B-cells with myeloma cells.
- The hybrid cell, which is produced as the result of this fusion, is called a hybridoma.
- This hybridoma possesses the immortal growth properties of the myeloma cell and the antibody-secreting property of the B-cell.
The fusing agent can be a defective virus (Sendai virus that characteristically causes cell fusion) or chemicals like polyethylene glycol.
The steps to produce the monoclonal antibodies are as follows
Isolation of B-lymphocytes
The isolation of B-lymphocytes takes place from the spleen of an animal like a Mouse.
This animal is previously immunized with the antigen against the desired monoclonal antibodies.
The immunization of animals is achieved by injecting the antigen with a suitable adjuvant (non-antigenic preparation known to stimulate an immune response). This may be repeated multiple times (booster doses of antigen).
Immunization enhances the population of B-lymphocytes that produce antibodies against the specific antigen used.
This is called clonal selection.
In clonal selection, the antigen reacts to the cell surface receptor of B-lymphocytes, leading to rapid proliferation.
This population of B-cells, which can produce antibodies of the same specificity, is called a clone. This whole process is called clonal selection.
Isolation of myeloma cells
The myeloma cells are fast-growing large cells of a hemopoietic portion of bone marrow.
It is capable of multiplying indefinitely. The myeloma cells are selected for only two features, which are as follows:
- These cells do not produce antibodies themselves.
- The cell contains a genetic marker (HGPRT –hypo xanthine phosphor ribosyl transferase), which permits an early solution of the resulting hybrid cells.
The myeloma cells are taken into account for the production of monoclonal antibodies.
Self-fusion
The next step is the fusion of HGPRT cells and B-lymphocytes. After the fusion of these two, the mixture is produced, which is treated further with PEG (polyethylene glycol).
The cell mixture is shaken well for 3 minutes. PEG brings the cells together and induces fusion.
The resulting cell population is the fusion unit of hybrid cells, which is called a hybridoma. i.e., myeloma cells and B-lymphocytes.
Selection of hybridoma cells
The resultant cell population is now cultured or cultivated in the HAT medium (the HAT medium is supplemented with hypoxanthine aminopterin thymidine).
The unfused myeloma cells can’t grow in the mixture because they lack HGPRT and thus cannot replicate.
The myeloma cells that contain HGPRT can only grow and replicate henceforth.
The hybridoma cells are able to grow indefinitely in the media because the spleen cell partner supplies HGPRT, and the myeloma partner has traits that make it immortal, similar to a cancer cell.
Then, the cultures are screened well for the selection of hybrids producing antibodies that are specific for the immunizing antigen.
The B-cells do not grow for a long period and eventually die due to a shorter lifespan.
The HGPRT myeloma cells are unable to divide in the HAT medium due to aminopterin because the HGPRT enzyme is responsible for purine synthesis.
However, aminopterin inhibits the purine biosynthesis in myeloma cells by alternate pathways.
Screening of hybridoma
The next step is the identification and isolation of hybridoma cells, which are specific to the antigen used for animals. It involves:
- The hybridoma cells are suspended suitably, diluted, and distributed into two microwells.
- The cell in each microwell is allowed to grow. The cells grow and secrete antibodies into the medium.
- The supernatant from each microwell is sampled for the presence of antibodies specific to the antigen studied.
Using one of the methods based on either precipitation or agglutination caused by the antibodies specific to the antigen.
Most times, ELISA is done in the process of extracting the monoclonal antibodies. This way, the monoclonal antibodies are produced.
In Vivo method
This method involves the following steps.
1. First, an animal, like a mouse, rabbit, etc., is immunized with a suitable antigen that corresponds to the desired monoclonal antibody we are interested in.
This is done by injecting antigens that are previously emulsified with some adjuvants like Freund’s adjuvant.
2. This leads to enhanced production of desired antibodies in the mouse body.
The immunization is done for a few weeks until the antibody concentration in the mouse blood reaches the desired level.
3. After several weeks, the blood test is done to see antibody titer using suitable techniques like ELISA or flow cytometry, etc., and is obtained from the mouse spleen.
4. Then, the obtained monoclonal antibodies are fused with a cancer cell (i.e., myeloma, not just tumor) as they are immortal and can divide indefinitely.
5. So, the fused cell grows indefinitely to produce a huge number of monoclonal antibodies. The bunch of fused cells is called a hybridoma.
6. These formed tumor cells are injected into the mouse peritoneal cavity or grown in vitro by tissue culture technique.
8. On injection into the mouse peritoneal cavity, the cell grows rapidly and releases in the form of liquid into the abdomen, which appears as bulged fluid bags (ascites).
9. These monoclonal antibodies from ascites are extracted to harvest the formed antibodies.
Another method is growing these hybridoma cells in vitro, but it is not easy and also is more expensive than the mouse method.
But sometimes, the mouse may experience pain irritation due to ascites. Then, they go for the in-vitro cell culture technique.
Application of monoclonal antibodies
Monoclonal antibodies find their application in diagnosis, imaging, and therapeutic agents in clinical medicine.
Such hybridoma–derived monoclonal antibodies are becoming increasingly important in diagnostic areas.
For example, in cancer therapy, monoclonal antibodies can be used directly to attack and destroy tumor cells.
They can be labeled with radioactive isotopes to locate tumors and to deliver specifically lethal doses of radiation to inaccessible tumors.
They can be used to deliver anticancer drugs to tumor cells in a similar manner.
Monoclonal antibodies vs. polyclonal
| Features | Monoclonal | Polyclonal |
|---|---|---|
| Source | Derived from single homogenous parent cell line. | Obtained as a mixture of antibodies where each is secreted from different B-cell lines. |
| Target | One single epitope or antigen of pathogens neutralizes them | Polyclonal antibodies have important but limited applications, like treating transplant rejection. |
| Technology | They require advanced technology to produce. | They can be produced with ease, in an inexpensive way, and also in a short time. |
| Application | One single epitope or antigen of pathogens neutralizes them | Monoclonal antibodies are widely used for the treatment of cancer, cardiac disorders, infections, and autoimmune disorders. |
| Drawbacks | Expensive | Monoclonal antibodies are widely used for the treatment of cancer, cardiac disorders, infections, autoimmune disorders. |
Do monoclonal antibodies replicate themselves within the body of a patient who received them — or continually stimulate other appropriate immune system response(s)? If not, does that then mean that the patient must receive periodic continued injections until the totality of the mAbs have destroyed or disabled the target molecules/cells of the therapy? (therein being a very significant difference between mAb therapy and vaccination)
Hi Larry, as per my understanding, monoclonal antibodies do not replicate in the body once administered. Hence, they need to be given repeatedly with caution and may require plasma level monitoring.
Vaccination help the body generate its own antibodies. When the body immune system is weak, Mab’s are preferred.
I think you have a bit of a gap in your understanding of antibodies. Go back to basics. A certain cell type of the immune system, the so-called B-cell, has the capacity, when activated, to produce a protein molecule called an antibody which has great specificity for combining with (and thus neutralizing) foreign entity (such as a bacterial cell or virus) a particular part of the foreign entity (the so-called antigen).
Antibodies DO NOT replicate themselves. Like any other protein product, they are produced by particular cells via the process of protein synthesis. The B-cells of the immune system secrete antibodies.
If you want to really understand this somewhat complex topic, I suggest you learn some basics.