Hemostasis is a series of overlapping processes intended to stop the bleeding during an injury to the blood vessel. It occurs in 4 stages as
- Vasoconstriction
- Platelet plug formation
- Coagulation
- Fibrinolysis
The process begins within 15 seconds after the injury. The platelets, which are a type of blood cells, play a vital role in it.
Vasoconstriction
In these stages, the injured blood vessel’s channel gets narrow so as to minimize the blood flow.
When the blood vessel is damaged, the thrombocytes flowing in the blood adhere to the damaged surface. These platelets get sticky and lead to further aggregation of platelets.
Since the platelets have serotonin inside them, they release it at the site of aggregation. This serotonin constricts the blood vessel intended to slow the flow of blood.
Besides this, the damaged vessel tissue also releases other vasoconstricting agents like thromboxane.
Plug formation by platelets
The sticky platelets adhere to each and release adenosine diphosphate (ADP).
This ADP acts as a chemotactic trigger to attract more platelets to the injured site. The thrombocytes flowing in the bloodstream stick to those already adhered at the site of injury.
Many thrombocytes arrive at the injured site due to a positive feedback system to form a platelet plug or seal.
This plug formation occurs in 6 minutes and prevents further leakage of blood from the injured site.
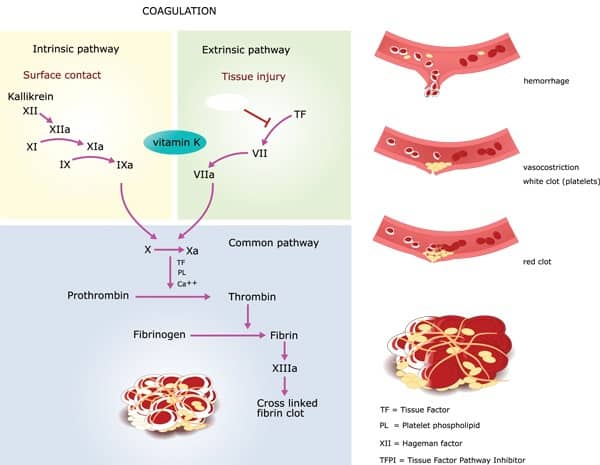
Coagulation
In this stage, another layer of the cover is formed on the previous platelet plug formed.
Here the plug is stabilized by the addition of insoluble fibrin threads over the plug.
This process involves 12 factors that go on to the formation of a prothrombin activator. The factors are termed clotting factors and are listed below.
| Factor | Name |
| I | Fibrinogen |
| II | Prothrombin |
| III | Thromboplastin (Tissue factor) |
| IV | Calcium |
| V | Labile factor, (Proaccelerin, AC-globulin) |
| VII | Stable factor (proconvertin) |
| VIII | Antihemophilic factor A, (antihaemophilic globulin -AHG) |
| IX | Christmas factor (plasma thromboplastin component-PTA), antihemophilic factor B |
| X | Stuart Prower factor |
| XI | Plasma thromboplastin antecedent (PTA), antihemophilic factor C |
| XII | Hageman factor |
| XIII | Fibrin stabilizing factor |
This prothrombin activator activates the enzyme thrombin which converts fibrinogen into insoluble fibrin threads.
These fibrin threads lie on the platelet plug in three-dimensional network format and further stabilize the blood clot.
The pathway of prothrombin activation is possible by two methods like
a) The extrinsic pathway
b) The intrinsic pathway.
The extrinsic pathway is faster and gets activated within seconds of tissue damage. The thromboplastin is released by damaged tissue which goes on to initiate coagulation.
The intrinsic pathway is slower and acts in 3 to 6 minutes. This is initiated when the blood gets in contact with damaged blood vessel inner walls. The platelets adhere to the endothelium the blood vessel’s inner wall.
Once the clot is formed, the platelets gradually contract and ooze out the serum. This leads to shrinkage of the clot with clear fluid on the surface.
As the clot retracts (shrinks) the edges of damaged blood vessel tissue are pulled together leading to the closure of the hole.
Fibrinolysis
This is a healing process of the damaged blood vessel. This phase begins with the breakdown of the clot. The clot is broken down by the enzyme plasmin which is an activated form of plasminogen. This plasmin converts insoluble fibrin to soluble form which is removed by phagocytosis. The healing process continues after the clot is removed until the restoration of blood vessel integrity.